Topical Calcipotriol for a Giant Wart
Matilda Bylaite and Thomas Ruzicka
Department of Dermatology, Heinrich-Heine-University Duesseldorf, Duesseldorf, Germany
History
A 41-year-old man presented with a painful, prominent, hyperkeratotic, periungual wart on his right fifth toe. It developed soon after local trauma and has been enlarging for the last 4 years. The wart has been unsuccessfully treated with various topical preparations and cryotherapy. He was otherwise healthy and was not taking any current medications. There was no history of an immunodeficiency. Clinical Findings
Physical examination revealed a solitary, 30 mm in diameter, thick, hyperkeratotic, verrucous, yellowish, periungual painful plaque localized on the lateral aspect of the right fifth toe with resultant nail deformity (Fig. 1).
| Fig. 1. Giant verruca vulgaris. Large, painful, hyperkeratotic periungual wart is present on the fifth toe. |
 |

  |
Histopathology
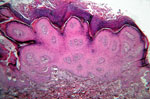
The histopathological findings of lesional skin biopsy showed characteristic features of verruca vulgaris (Fig. 2). One could observe acanthotic epidermis with hyperkeratosis, parakeratosis and papillomatosis. Vacuolated cells with small eosinophilic granules and basophilic keratohyaline granules were noticed in the upper epidermis.
| Fig. 2. Giant verruca vulgaris (HE, x 40). |
 |

  |
Examination and Laboratory Findings
Laboratory tests were within normal limits. A potassium hydroxide examination of the scales and nail material was negative for hyphae. Diagnosis
A clinical diagnosis of a giant recalcitrant verruca vulgaris was established. Therapy and Course
The patient refused both surgical excision and laser therapy. We decided therefore to treat him with topical calcipotriol ointment (50 µg/g) twice daily for a 3-month period. Orthopedic decompression and paring of the wart was regularly performed during the treatment. The wart decreased in size within the first month. The treatment has been continued without any local or systemic adverse events. At 5-month follow-up visit, the skin of the toe and nail fold was free from the wart (Fig. 3). No recurrence was seen in the next 2 months. There was no change of serum Ca2+ during the treatment period.
| Fig. 3. Complete clinical regression of the wart after topical treatment with calcipotriol. |
 |

  |
Discussion
Common warts (verrucae vulgares) are hyperkeratotic, benign epithelial tumors, which are caused by human papillomavirus (HPV), mainly by HPV type 1, 2, 4 and 57 (1), and most often presenting on the hands, arms and legs in children and adults. Not only viral type, but also environmental and host factors may influence the clinical appearance and localization of the warts (1). Development of periungual warts, as in our case, is usually provoked by trauma and maceration. Viral warts remain a therapeutic challenge for dermatologists and general practitioners. Usually, the treatment of warts is time consuming, expensive, and definitive cure is difficult to achieve. Patients are often frustrated by their large or multiple, recalcitrant and recurrent warts, and suffer for major cosmetic, functional and social discomfort (2). To date, a long list of therapeutic modalities has been used. Unfortunately, no treatment is ideal and warts are often recalcitrant against the various treatment options and combinations, especially in immunosuppressed patients. Keratolytic agents are usually the first-line approach. Other traditional treatments that are destructive and painful, and which might cause scarring include cryotherapy, surgical excision, electrodesiccation, infrared coagulation, laser vaporization, as well as photodynamic therapy and localized heating (1, 3, 4). Topical agents, which interrupt the cell division (podophyllotoxin, 5-fluorouracil, bleomycin, intralesional or systemic interferon and retinoids) or modify the immune response (cimetidine and topical 5% imiquimod) have also been used for the therapy of viral warts (1, 3). Recently, Egawa and Ono reported three immunocompromised patients with recalcitrant warts successfully treated with a vitamin D3 derivative, mexacalcitol, using a half-day occlusive dressing technique (5). To our knowledge, this was the only report where vitamin D3 derivatives have been used for the treatment of warts. Synthetic vitamin D3 derivatives have been shown to be effective in psoriasis and other disorders of abnormal epidermal growth and differentiation, including ichthyosis, palmoplantar keratosis and pityriasis rubra pilaris (6, 7). This supports the concept that vitamin D3 derivatives have an effect on epidermal cell differentiation and proliferation, inhibition of angiogenesis, and modulation of cytokine production (8, 9). We describe a patient with a giant recalcitrant periungual wart who was successfully treated with the vitamin D3 derivative calcipotriol. The treatment was well tolerated by our patient, and no adverse events were observed. The giant periungual wart with long duration and resistance to previous treatments, as seen in our case, is less likely to resolve spontaneously. We conclude that topical treatment with vitamin D3 derivatives may be a safe and effective therapy option for patients with recalcitrant warts. Further randomized placebo-controlled clinical trials could verify whether vitamin D3 derivatives are efficient in treating warts. References
1. Sterling J.C., Handfield-Jones, S., Hudson, P.M. Guidelines for the management of cutaneous warts. Br J Dermatol 2001, 144: 4-11.
2. Ciconte, A., Campbell, J., Tabrizi, S., Garland, S., Marks, R. Warts are not merely blemishes on the skin: a study on the morbidity associated with having viral cutaneous warts. Australas J Dermatol 2003, 44: 169-73.
3. Hengge, U.R, Esser, S., Schultewolter, T. et al. Self-administered topical 5% imiquimod for the treatment of common warts and molluscum contagiosum. Br J Dermatol 2000, 143: 1026-31.
4. Tosti, A., Piraccini, B.M. Warts of the nail unit: Surgical and nonsurgical approaches. Dermatol Surg 2001, 27: 235-9.
5. Egawa, K., Ono, T. Topical vitamin D3 derivatives for recalcitrant warts in three immunocompromised patients. Br J Dermatol 2004, 150: 374-6.
6. Mason, J., Mason, A.R., Cork, M.J. Topical preparations for the treatment of psoriasis: A systemic review. Br J Dermatol 2002, 146: 351-64.
8. Osborne, J.E., Hutchinson, P.E. Vitamin D and systemic cancer: Is this relevant to malignant melanoma? Br J Dermatol 2002, 147: 197-213.
7. Van de Kerkhof, P.C., Wittenhorst, M., Gerritsen, M.J., de Jong, E.M., Lucker, G.P., Steylen, P.M. Possible indications for vitamin D3 analogues in conditions other than psoriasis vulgaris. J Dermatol Treat 1996, 7: 195-8.
9. Bikle, D.D., Gee, E., Pillai, S. Regulation of keratinocyte growth, differentiation, and vitamin D metabolism by analogs of 1,25-dihydroxy vitamin D. J Invest Dermatol 1993, 101: 713-8. |