Eruptive Xanthomas
Matilda Bylaite and Thomas Ruzicka
Department of Dermatology, Heinrich-Heine-University Duesseldorf, Duesseldorf, Germany
History
A 34-year-old man was seen in our outpatient department for an asymptomatic, yellowish eruption on the extensor surface of his extremities and the back of his neck. The lesions appeared suddenly and increased in number over a period of 2 months. His past medical history was not remarkable. He denied any systemic symptoms, and lately was not taking any medications. There was no family history of similar eruption, hyperlipoproteinemia, diabetes, cardiovascular disease or sudden death. Clinical Findings
Physical examination disclosed mild obesity. Numerous, grouped, small, 2-4 mm in diameter, dome-shaped, non-confluent, yellowish-erythematous papules were symmetrically distributed over the nape of his neck and extensor surfaces of forearms, elbows, thighs, and knees (Figs. 1-3). No lesions were noted on his eyelids, mucous membranes, palms or Achilles tendons. No other skin abnormality was noticed besides mild keratosis pilaris. The liver and spleen were not palpable.
| Fig. 1. Numerous eruptive xanthomas are distributed over extensor surfaces of patient's extremities. |
 |

  |
| Fig. 2. Close-up view of discrete yellowish-erythematous papules and mild keratosis pilaris. |
 |

  |
| Fig. 3. A yellowish "lipoid" aspect was seen on diascopy of xanthomatous papules. |
 |

  |
Histopathology
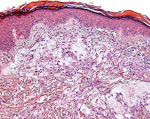
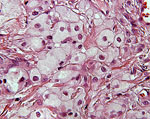
Three biopsy specimens from discrete yellow papules were obtained. Histological examination revealed collections of foamy histiocytes, so called xanthoma cells, within the upper and middle dermis, mild fibrosis and sparse infiltrate of lymphocytes and few neutrophils (Figs. 4, 5). The epidermis showed mild hyperkeratosis, parakeratosis and acanthosis. The histological findings were similar in all three specimens, and were consistent with eruptive xanthomas.
| Fig. 4. Eruptive xanthoma with characteristic foamy histiocytes and inflammatory infiltrate in reticular dermis (HE x100). |
 |

  |
| Fig. 5. The xanthoma cells have abundant foamy-appearing cytoplasm and small nuclei (HE x400). |
 |

  |
Examination and Laboratory Findings
Complete blood count, glucose level, as well as liver, pancreas and renal function studies were within normal limits. Standard tests for syphilis were nonreactive. Lipid studies showed a normal level of serum cholesterol (95 mg/dl; normal <200 mg/dl), and markedly elevated levels of serum triglycerides (4600-3620 mg/dl; normal <200 mg/dl). Ultracentrifugation analysis and electrophoresis of lipoproteins were not performed. Diagnosis
A diagnosis of eruptive xanthomas due to hypertriglyceridemia was made. Therapy and Course
A low-fat, low-calorie diet was suggested to our patient. Within one month, without any additional drug therapy, the cutaneous lesions resolved spontaneously, and the serum triglyceride levels decreased. However, we referred our patient to the internist for further systemic investigation. Discussion
Xanthomas are known as indicators of a hyperlipidemic state and lipid metabolism dysfunction. In 1965, Fredrickson and Lees proposed a classification of familial hyperlipoproteinemia, which is still widely used (1). The division into five types of hyperlipoproteinemia was based on paper electrophoresis. Type I was classified as hyperchylomicronemia, type II as hyper-ß-lipoproteinemia, type III as a combination of both hyper-ß- and pre-ß-lipoproteinemia, type IV as hyper-pre-ß-lipoproteinemia, and, the last, type V as hyperchylomicronemia in combination with hyper-pre-ß-lipoproteinemia. Moreover, it was proved that different types of hyperlipoproteinemia had different clinical manifestations, responses to therapy and diet, and different genetic aspects (1, 2). Estimation of lipoprotein content of the serum by ultracentrifugation definitively confirmed above-mentioned findings (1, 2). Generally, xanthomas present as xanthelasma palpebrarum, tuberous xanthoma, tendinous xanthoma, striated xanthoma, plane and generalized xanthoma and finally, eruptive xanthoma. Eruptive xanthomas reflect hypertriglyceridemia, chylomicronemia and high plasma concentrations of very low-density lipoproteins (VLDL). These abnormalities are seen in type I, III, IV and V of hyperlipoproteinemias (1-3). Eruptive xanthomas also occur in diseases where insulin deficiency and acquired lipoprotein lipase deficiency leads to hypertriglyceridemia. These secondary hyperlipidemias, commonly resulting from uncontrolled diabetes mellitus, hypothyroidism, nephrotic syndrome, dysproteinemias, pancreatitis, liver disease and alcoholism should be ruled out (1, 3, 4). A list of drugs, including systemic steroids, thyroid hormones, progestational hormones and large doses of aspirin may also affect plasma lipid levels (4). Furthermore, eruptive xanthomas have been reported in association with medications, such as intravenous miconazole (6), isotretinoin (7), indomethacin and recently, olanzepine (8) and retroviral protease inhibitors, specifically ritonavir (9). Nevertheless, Caputo et al. reported a patient with eruptive xanthomas and normal plasma lipids (10). Clinically, eruptive xanthomas appear suddenly as small, dome-shaped, pink or yellow-orange papules, sometimes with an erythematous halo around the base, especially over pressure points, on extensor surfaces of the extremities and buttocks (5). However, the lesions can be found on all cutaneous surfaces, including mucous membranes (3), and also in combination with other xanthomatous lesions. The Köbner phenomenon may be present (11). Although eruptive xanthomas are generally asymptomatic, on occasion they may be itchy or tender. In addition to skin findings, because of high triglyceride levels, patients may manifest acute pancreatitis and lipemia retinalis. Histologically, eruptive xanthomas show a characteristic picture as described above. Complete laboratory and internal examination of the patient with eruptive xanthomas or other types of xanthomas should be performed to rule out the reason for hyperlipidemic state. Estimations of plasma lipids, and, if available, centrifugation and plasma lipoprotein electrophoresis could give an indication of the underlying cause (1). The therapeutic approach is very individual. Treatment is usually successful and includes a low-fat and low-calorie diet, and, if required, antihyperlipidemic drugs such as clofibrates, cholestyramine, dextrothyroxine or nicotinic acid (3, 4). Correction of secondary hyperlipidemias or underlying diseases is mandatory. The skin lesions generally regress spontaneously when plasma lipid concentration becomes lower (3). However, recurrences occur if the treatment is discontinued. In our patient, eruptive xanthomas developed in association with a marked elevation of serum triglycerides probably due to excessive fat and carbohydrate intake on a genetic background. After initiation of low-fat and low-calorie diet, his cutaneous lesions resolved rapidly within a month. As dermatologists, we should be aware that eruptive xanthomas might be the first manifestation of an underlying hyperlipidemic state, which is a risk factor for arteriosclerotic vascular disease and pancreatitis. Therefore, a prompt identification of eruptive xanthomas and their potential association with systemic disorders leads to effective and immediate treatment. References
1. Fredrickson, D.S., Lees, R.S. A system for phenotyping hyperlipoproteinemia. Circulation 1965, 31: 321-7.
2. Polano, M.K. Xanthomatosis and hyperlipoproteinemia. A review. Dermatologica 1974, 149: 1-9.
3. Cornelius, C.E. III. Disappearance of eruptive xanthoma following carbohydrate restriction. Arch Dermatol 1967, 96: 45-50.
4. Fleishmajer. R., Dowlati, Y., Reeves, J.R.T. Familial hyperlipidemia diagnosis and treatment. Arch Dermatol 1974, 110: 43-50.
5. Parker, F. Xanthomas and hyperlipidemias. J Am Acad Dermatol 1985, 13: 1-30.
6. Barr, R.J., Fujita, W.H., Graham, J.H. Eruptive xanthomas associated with intravenous miconazole therapy. Arch Dermatol 1978, 114: 1544-5.
7. Dicken, C.H., Connolly, S.M. Eruptive xanthomas associated with isotretinoin (13-cis-retinoic acid). Arch Dermatol 1980, 116: 951-2.
8. Chang, H.Y. et al. Eruptive xanthomas associated with olanzapine use. Arch Dermatol 2003, 139: 1045-8.
9. Geyer, A.S. et al. Eruptive xanthomas associated with protease inhibitor therapy. Arch Dermatol 2004, 140: 617-8.
10. Caputo, R., Marcello, M. et al. Normolipemic eruptive cutaneous xanthomatosis. Arch Dermatol 1986, 122: 1294-7.
11. Goldstein, G.D. The Koebner response with eruptive xanthomas. J Am Acad Dermatol 1984, 10: 1064-5. |