Acrodermatitis Chronica Atrophicans
Matilda Bylaite and Thomas Ruzicka
Department of Dermatology, Heinrich-Heine-University Duesseldorf, Duesseldorf, Germany
History
A 73-year-old female patient presented with a 9-month history of inflamed and slowly enlarging livid-reddish skin lesions on her right knee and the dorsa of the right foot. The skin disease had begun approximately 1 year earlier, when the patient developed on the same extremity a map-like marginally expanding erythematous skin rash which vanished without therapy after 1 month. Within the next month, she noted swelling and pronounced pain in her right foot, and later markedly increased pain in her right knee. Since the patient suffered from gonarthrosis, the symptoms were considered as an exacerbation of degenerative joint disease. However, inflammatory skin changes gradually evolved over the symptomatic joints. Moreover, she lived in rural area, and recalled repeated tick bites. Additionally, she had varicose veins, and complained of low-back pain and hypertension. For a chronic pain syndrome she was regularly taking analgesics and antiinflammatory medication. Clinical Findings
Clinical examination revealed two bluish-red and slightly edematous plaques with indistinct borders and approximately 10 cm in diameter on the right knee and dorsum of the right foot including ankle area (Figs. 1 and 2). On closer examination, the lesions were smooth and atrophic, and had a ‘crumpled tissue-paper’ appearance. The underlying joints were swollen, warm and tender on palpation. Two enlarged lymph nodes were palpable in the right groin. Multiple, dark-brown discrete macules were scattered over her face and extremities. The network of varicose veins was prominent on the lower legs.
| Fig. 1. Acrodermatitis chronica atrophicans (ACA): a bluish-red inflamed plaque with a slight cutaneous atrophy on the right knee. |
 |

  |
| Fig. 2. ACA plaque on the right ankle area. |
 |

  |
Histopathology
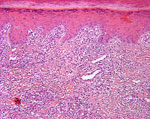
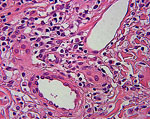
The histological examination of a biopsy of both lesions disclosed hyperkeratosis and atrophic epidermis, edema in the upper and middle dermis with a rich infiltration of lymphocytes and plasma cells, compatible with a diagnosis of acrodermatitis chronica atrophicans (Figs. 3 and 4).
| Fig. 3. Histopathology of ACA biopsy from the right knee shows a moderate atrophic epidermis, thickened underlying dermis and a chronic inflammatory infiltrate rich in plasma cells (HE x100). |
 |

  |
| Fig. 4. Dermal infiltration around dilated vessels with lymphocytes and plasma cells in ACA (HE x400). |
 |

  |
Examination and Laboratory Findings
Full blood count, erythrocyte sedimentation rate, renal and liver function tests were normal. Treponema pallidum hemagglutination assay (TPHA) was negative. There were slightly elevated IgM (25; N: <20) and moderately elevated IgG (170; N: <20) serum titers to Borrelia determined by ELISA. A Western blot was negative. Nerve-conduction studies revealed a subclinical peripheral sensory neuropathy of the lower legs. X-ray and skeletal scintigraphy showed osteoarthrotic changes in most of the joints. There were no significant changes in echocardiography. Diagnosis
Based on history, clinical appearance, histopathological findings and elevated serum IgG antibodies to Borrelia, a diagnosis of acrodermatitis chronica atrophicans was established. Therapy and Course
The patient was treated with intravenous ceftriaxone (2 g daily) for 3 weeks. Additionally, she received nonsteroidal antiinflammatory drugs and analgesics. Locally, fluticasone propionate ointment was applied twice daily. After 2 weeks of therapy, her condition progressively improved. Pain and swelling in the joints decreased by the end of the treatment. There was a marked reduction of the skin inflammation, and the lesions gradually began to fade, but the atrophy remained (Fig. 5).
| Fig. 5. ACA lesion on the knee after treatment with intravenous ceftriaxone. |
 |

  |
Discussion
Lyme borreliosis (LB) is a multistage disease that affects the skin, joints, cardiovascular and nervous systems. The disease is caused by Borrelia burgdorferi sensu lato infection transmitted by Ixodes ricinus tick bites (1). Various species of B. burgdorferi sensu lato differ in geographic distribution (2), and preferentially affecting various organs show distinct clinical manifestations of Lyme disease (3). Acrodermatitis chronica atrophicans (ACA) is a late cutaneous manifestation that occurs in up to 10% of patients with LB (4), usually being caused by B. afzelii (3). The condition was first described in 1883 by Buchwald (5), but only in 1902 was the name of ACA given by Herxheimer and Hartman (6). It was observed that ACA is common in central and northern Europe and rarely occurs in the U.K., America, Australia and Asia (7). The patients often do not recall a tick bite. The disease presents predominantly in women (70%) over 40 years who are usually country dwellers. About 20% of the patients have a history of an untreated erythema migrans, generally on the same extremity where ACA lesions developed later (8). Typically, single or multiple bluish-red discoloration or infiltrated plaques insidiously develop on extensor surface of extremities. Inflammatory ACA lesions may persist for years gradually becoming atrophic, wrinkled and paper-like with prominent vessels. Firm, skin-colored or bluish-red, not tender nodules or indurated bands may also develop over the knees and elbows as well as ulnar region. Therefore, migrating and/or intermittent pains due to impact against bony prominences underlying ACA skin lesions are frequent. Peripheral neuropathy is present in more than 50% of patients with ACA. Subluxations/luxations of small joints and periosteal thickening of bones have been reported underneath the skin lesions in patients with long-standing ACA. Systemic manifestation of LB and also fatigue, personality changes or emotional disturbance may accompany ACA. Morphea of the trunk and lichen sclerosus et atrophicus (both genital and extragenital) have been associated with ACA (7, 9). Basal cell carcinoma (10) and squamous cell carcinoma (11) may develop in the atrophic skin of a patient with ACA. Lymphoma has been reported in nonaffected skin (12). However, the clinical recognition of ACA may be difficult. Commonly, the disease is mistaken with venous stasis or lymphedema, and sometimes dermatomyositis. Fibrotic nodules may be confused with rheumatic nodules or gouty tophi. Clinically suspected inflammatory ACA lesions should be verified by the histopathologic pattern and by elevated serum titers of IgG antibodies to B. burgdorferi. The diagnosis may be confirmed also by spirochetal cultivation, as borreliae may still be present in the skin even after more than 10 years of ACA. Other laboratory testing of LB includes antibody detection using ELISA with whole extracts or recombinant chimeric borrelia proteins, Immunoblot and polymerase chain reaction (PCR). Doxycycline and ceftriaxone are the most commonly used antibiotics in the various stages of Lyme borreliosis. Oral or systemic antibiotics should be given for 3 weeks in standard doses. Improvement occurs gradually, several weeks after the course of treatment. The peripheral neuropathy associated with ACA develops in some patients despite antibiotic treatment. Jarish-Herxheimer reactions occur in 10% of treated patients. However, once atrophy has developed, there is usually little response to treatment. Thus, follow-up in regular intervals for the development of possible malignancies in atrophic skin is recommended. Lyme borreliosis may be prevented by avoiding endemic areas, keeping the skin covered and using tick repellents. Frequent skin inspections for early detection and removal of ticks within 24 hours are suggested. Laboratory tests after a tick bite are not recommended, nor is prophylactic treatment with antibiotics. Recently developed vaccines remain under investigation whether they are effective and capable of preventing infection with B. burgdorferi (12). Here we describe a patient with acrodermatitis chronica atrophicans that fulfills the criteria for chronic cutaneous manifestation of borreliosis. Whether our patient had been suffering from allodynia or pain due to osteoarthrosis was difficult to distinguish. Even though the inflammatory changes of ACA rapidly responded to the treatment with ceftriaxone, slight atrophy was still seen after 1 month. References
1. Steere, A.C. Lyme disease. N Engl J Med 1989, 321: 586-96.
2. Baranton, G., Marti Ras, N., Postic, D. Molecular epidemiology of the aetiological agents of Lyme borreliosis. Wiener Klinische Wochenschrift 1998, 110: 850-5.
3. Van Dam, A.P., Kuiper, H., Vos, K. et al. Different genospecies of Borrelia burgdorferi are associated with distinct clinical manifestations of Lyme borreliosis. Clin Infect Dis 1993, 17: 708-17.
4. Leslie, T.A., Levell, N.J., Cutler, S.J. et al. Acrodermatitis chronica atrophicans: a case report and review of the literature. Br J Dermatol 1994, 131: 687-93.
5. Buchwald A. Ein Fall von diffuser idiopathischer Hautatrophie. Vjschr Derm 1883, 15: 553-6.
6. Herxheimer, K., Hartman, K. Über Acrodermatitis chronica atrophicans. Arch Dermatol (Berl) 1902, 61: 57-76.
7. Coulson, I.H. Acrodermatitis chronica atrophicans with coexisting morphoea. Br J Dermatol 1989, 121: 263-9.
8. Åsbrink, E. Erythema chronicum migrans Afzelius and acrodermatitis chronica atrophicans. Early and late manifestations of Ixodes ricinus-borne Borrelia spirochetes. Acta Derm Venerol (Stockh) 1985, 118(Suppl): 1.
9. Ramelet, A.A. Association of acrodermatitis chronica atrophicans and morphoea. Dermatologica 1987, 175: 253-6.
10. Lagerholm, B., Molin, L., Gip, L. Basal cell carcinoma in association with acrodermatitis chronica atrophicans Herxheimer. Acta Dermatovener (Stockh) 1970, 50: 218.
11. Garbe, C., Stein, H., Dienemann, D., Orfanos, C.E. Borrelia burgdorferi-associated cutaneous B cell lymphoma. J Am Acad Dermatol 1991, 24: 584-90.
12. Steere, A.C., Sikand, V.K., Meurice, F. et al. Vaccination against Lyme disease with recombinant Borrelia burgdorferi outer-surface lipoprotein A with adjuvant. N Engl JMed 1998, 339: 209-15. |