Radiation-Induced Angiosarcoma
Matilda Bylaite and Thomas Ruzicka
Department of Dermatology, Heinrich-Heine-University Duesseldorf, Duesseldorf, Germany
History
A 48-year-old woman was referred to our clinic with painless bluish-brown lesions on her left forearm that developed over a period of 4-5 months at the site of previous irradiation. She was approximately 3 years old when radiotherapy was performed for hemangiomas on her left forearm and the right gluteal area. Thereafter, the hemangiomas completely disappeared leaving signs of local radiation dermatitis. A recurrence of hemangioma or angiosarcoma was suspected clinically. Although she suffered from postoperative hypothyroidism, uterine myoma and ovarian cysts, she was otherwise in a good health and her family history was unremarkable. Clinical Findings
On examination, ill-defined, livid-brown, 0.7 cm and 0.3 cm in diameter flat nodules were located on her left lateral forearm at the site of slightly atrophic and poikilodermic skin (Fig. 1). The nodules were firm to the touch and asymptomatic. Regional lymph nodes were not enlarged. On her right gluteal area, late-stage radiation dermatitis was observed. Additionally, multiple angiomas and seborrheic keratoses were scattered over her trunk.
| Fig. 1. Radiation-induced cutaneous angiosarcoma presenting as two livid-brown nodules on the left forearm. |
 |

  |
Histopathology
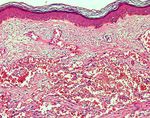
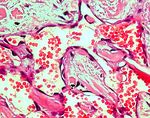
A skin biopsy specimen taken from the nodule revealed a diffusely infiltrating irregular vascular proliferation dissecting the collagen bundles of the deep and superficial dermis (Fig. 2). Neoplastic blood vessels were lined by atypical endothelial cells with eosinophilic cytoplasm and large atypical nuclei (Fig. 3). Proliferating endothelial cells overlapped and protruded into the vascular lumen which contained numerous erythrocytes. At the base of the tumor, an infiltrate of lymphocytes was present. These findings were diagnostic for angiosarcoma.
| Fig. 2. Angiosarcoma: a diffusely infiltrating vascular proliferation dissecting the collagen bundles of the dermis (HE, x100). |
 |

  |
| Fig. 3. Bizarre vascular spaces lined by atypical endothelial cells and erythrocytes in the lumen (HE, x400). |
 |

  |
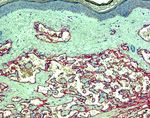
Immunohistochemistry performed with CD31 and CD34 (Fig. 4) showed a diffuse staining of tumor cells and normal dermal vascular structures, confirming the endothelial nature of the neoplasia. Factor VIII-related antigen showed rather focal staining pattern of neoplasm.
| Fig. 4. Positive immunostaining with CD34 of tumor cells and normal dermal vascular structures (x100). |
 |

  |
The histopathological examination of the biopsy from the right gluteal area revealed radioderma without any malignant signs. Examination and Laboratory Findings
Routine blood tests were within normal ranges. Staging examination, including lymph node sonography, thyroid, chest and abdomen computer tomography, and full skeletal scintigraphy provided no evidence of metastatic disease or alteration of underlying bone structures. Diagnosis
Based on patient’s history, clinical and histopathological findings, a diagnosis of radiation-induced cutaneous angiosarcoma of the left forearm was established. Therapy and Course
The tumor was excised in two steps with large lateral margins including the fascia. The wound was closed with a full-thickness skin graft from her right upper leg. Micrographic margin controls showed residual tumor tissue in the deep borders close to the bone, postoperative irradiation was therefore initiated. Radiotherapy with an electron beam using 33 fractionated doses of 2 Gy for up to total of 60 Gy was performed. Regular follow-up for possible recurrences and metastatic disease was recommended. Discussion
Angiosarcoma (AS, malignant hemangioendothelioma) is a rare, highly malignant vascular tumor with a tendency to extend rapidly and metastasize early. Its etiology and exact pathogenesis remain unclear. Angiosarcoma represents about 2% of all soft tissue sarcomas, preferably appearing in the skin and superficial soft tissue (1); however, one quarter of these tumors occur also in internal organs, such as liver, breast, bone or spleen (2). Cutaneous angiosarcomas may clinically present in several forms. Classically, angiosarcomas occur predominantly on the face and scalp mainly in elderly men (3). They appear as multifocal bruise-like lesions or resemble rosacea and rhinophyma (4). Second in frequency presentation of angiosarcoma is observed in areas of long-lasting chronic lymphedema that is mainly iatrogenic (in 90%). Commonly, it occurs in the upper extremities of postmastectomy patients with or without following radiotherapy as a component of the Stewart-Treves syndrome (5). Other causes of chronic edema such as congenital factors (6), trauma (7), recurrent cellulitis (8), idiopathic causes (1) or postsurgical obstruction are less often associated with angiosarcomas. Very rarely angiosarcomas develop as a result of previous radiation therapy. The following criteria characterize a radiation-induced angiosarcoma: (i) a history of irradiation, (ii) tumor development in the field of radiation or in the directly adjacent skin, (iii) a latency period of several years, and (iiii) a histological confirmation of AS. Usually, angiosarcomas occur in the skin or underlying soft tissue at sites of previous radiotherapy after a latent average period of 23 years in patients who received irradiation for benign conditions such as cutaneous hemangioma (9-11), hand eczema (12), sinusitis (13) and acne (14). A shorter interval (mean 12.3 years), probably due to higher doses of radiation, has been associated with malignant neoplasias, e.g., carcinoma of the cervix, endometrium, ovary, breast and Hodgkin’s disease (15). Angiosarcoma after previous radiation therapy for hemangioma was first described in 1950 (9), since then several additional cases have been reported. The clinical presentation of radiation-induced AS varies from case to case occurring as unilocal or often multifocal papulonodules, diffuse infiltrative plaques, and ulcerated lesions. Preexisting radiodermatitis of the involved area, as seen in our patient, has been described. Post-irradiation angiosarcoma demonstrates a histopathologic picture similar to that of other variants of cutaneous AS, showing numerous bizarre irregular vascular spaces lined by atypical prominent plump endothelial cells mainly with hyperchromatic nuclei, involving almost entire dermis and infiltrating the subcutaneous fat. Since angiosarcoma has a highly aggressive behavior, an early biopsy is essential to detect it in a stage when an adequate and early treatment might give a better outcome. Staging examination including computed tomography scan and scintigraphy is mandatory before and after treatment. Unfortunately, in many cases, the diagnosis of AS is delayed and the patients present when the tumor is large, extends into the subcutaneous tissue or, moreover, has already metastasized. The treatment of choice is complete excision with wide margins followed by micrographic controls. However, achieving negative margins is often impossible since angiosarcomas have the tendency to be multicentric, deeply invasive with ill-defined borders that histologically extend far beyond the clinical lesions. Usually, postoperative irradiation with high-energy electrons using doses of 60 Gy at 2 Gy per fraction is recommended as it may improve survival (1, 16). Radiation without surgery is of limited benefit (17). Chemotherapy has also been used with minimal success providing also only a palliative value. Response to treatment with paclitaxel, ifosfamide, liposomal doxorubicin as a single-agent or in combination with radiotherapy, interferon-alfa with oral 13-cis-retinoic acid has been reported by several authors. Unfortunately, these therapeutic approaches showed no prolonged survival benefit (18-20). Intralesional interferon alfa 2b and interleukin 2 have been also used (21). Regardless of aggressive treatment, the prognosis of angiosarcomas is generally poor with reported 5-year survival rates of 10% to 35% (1). Local recurrence and early lymphatic or hematogenous metastases are common, especially when the tumor is not completely excised (22). The most common sites of metastases are the lymph nodes, lungs, liver, bone and adrenal glands (23). In summary, we describe a case of angiosarcoma that manifested at a site of previous radiation therapy for hemangioma after 40 years of latent period. Cutaneous angiosarcomas as a late complication of irradiation should alert dermatologist for an early diagnosis for improved outcome, while the suspicious lesions are still limited in size, to avoid local relapse and metastasis by the aggressive behavior of this tumor. References
1. Mark, R.J., Poen, J.C., Tran, L.M., Fu, Y.S., Juillard, G.F. Angiosarcoma - a report of 67 patients and a review of the literature. Cancer 1996, 77: 2400-6.
2. Enzinger, F.M., Weiss, S.W. Malignant vascular tumors. In: Soft Tissue Tumors. 3rd ed. St Louis: Mosby, 1995: 641-77.
3. Holden, C.A., Spittle, M.F., Jones, E.W. Angiosarcoma of the face and scalp, prognosis and treatment. Cancer 1987, 59: 1046-57.
4. Aquila, L.I., Sánchez, J.L. Angiosarcoma of the face resembling rhinophyma. J Am Acad Dermatol 2003, 49: 530-1.
5. Stewart, F.W., Treves, N. Lymphangiosarcoma in postmastectomy lymphedema: a report of six cases in elephantiasis chirurgica. Cancer 1948, 1: 64-81.
6. Merrick, T.A., Erlandson, R.A., Hadju, S.I. Lymphangiosarcoma of congenitally lymphedematous arm. Arch Pathol 1971, 91: 365-71.
7. Sordillo, P.P., Chapmann, R., Hadju, S.I., Magill, G.B., Golbey, R.B. Lymphangiosarcoma. Cancer 1981, 48: 1674-9.
8. Azam, M., Saboorian, M.H., Bieligk, S., Smith, T., Molberg, K. Cutaneous angiosarcoma complicating morbid obesity. Arch Pathol Lab Med 2001, 125: 531-3.
9. McCarthy, W.D., Pack, G.T. Malignant blood vessel tumors: a report of 56cases of angiosarcoma and Kaposi’s sarcoma. Surg Gynecol Obstet 1950, 91: 465-82.
10. Costello, S.A., Seywright, M. Postirradiation malignant transformation in benign haemangioma. Eur J Surg Oncol 1990, 16: 517-9.
11. Caldwell, J.B., Ryan, M.C., Benson, P.M., James, W.D. Cutaneous angiosarcoma arising in the radiation site of a congenital hemangioma. J Am Acad Dermatol 1995, 33: 865-70.
12. Girard, C., Johnson, W.C., Graham, J.H. Cutaneous angiosarcoma. Cancer 1970, 26: 868-83.
13. Hodgkinson, D.J., Soule, E.H., Woods, J.E. Cutaneous angiosarcoma of the head and neck. Cancer 1979, 44: 1106-13.
14. Seo, I.S., Warner, T.F.C.S., Warner, J.S., Bennett, J.F. Cutaneous postirradiation sarcoma: ultrastructural evidence of pluripotential mesenchymal cell derivation. Cancer 1985, 56: 761-7.
15. Requena, L., Sangueza, O.P. Cutaneous vascular proliferations. Part III. Malignant neoplasms, other cutaneous neoplasms with significant vascular component, and disorders erroneously considered as vascular neoplasms. J Am Acad Dermatol 1998, 38: 143-75.
16. Sagar, S.M., Pujara, C.M. Radical treatment of angiosarcoma of the scalp using megavoltage electron beam therapy. Br J Radiol 1992, 65: 421-4.
17. Del Mar Saez de Ocariz, M., de la Barreda, F., Angeles, L.B. Angiosarcoma of the scalp. Int J Dermatol 1999, 38: 697-9.
18. Fata, F., O’Reilly, E., Ilson, D. et al. Paclitaxel in the treatment of patients with angiosarcoma of the scalp or face. Cancer 1999, 86: 2034-7.
19. Wollina, U., Fuller, J., Graefe, T., Kaattz, M., Lopatta, E. Angiosarcoma of the scalp: treatment with liposomal doxorubicin and radiotherapy. J Cancer Res Clin Oncol 2001, 127: 396-9.
20. Spieth, K., Gille, J., Kaufmann, R. Therapeutic efficacy of interferon alfa-2a and 13-cis retinoic acid in recurrent angiosarcoma of the head. Arch Dermatol 1999, 135: 1035-7.
21. Ulrich, L., Krause, M., Brachmann, A., Franke, I., Gollnick, H. Successful treatment of angiosarcoma of the scalp by intralesional cytokine therapy and surface irradiation. J Eur Acad Dermatol Venerol 2000, 14: 412-5.
22. Kacker, A., Antonescu, C.R., Shaha, A.R. Multifocal angiosarcoma of the scalp: a case report and review of the literature. Ear Nose Throat 1999, 78: 302-5.
23. Naka, N., Ohsawa, M., Tomita, Y. et al. Angiosarcoma in Japan: a review of 99 cases. Cancer 1995, 75: 989-96. |