Topical Tacrolimus is Effective in the Treatment of Lupus Erythematosus Tumidus
Matilda Bylaite and Thomas Ruzicka
Department of Dermatology, Heinrich-Heine-University Duesseldorf, Duesseldorf, Germany
History
A 47-year-old woman was referred to our clinic for evaluation of recurrent, asymptomatic, non-scarring erythematous lesions on her neck, both shoulders and right upper arm. The first papuloerythematous lesions appeared 3 years ago on her right cheek, back and décolleté. Exposure to sunlight exacerbated the lesions, but they were present also during the wintertime. The differential diagnosis included polymorphic light eruption, figurate erythema, pseudolymphoma and borrelial lymphocytoma. The diagnosis of lupus erythematosus was previously excluded, since the histological findings were not characteristic and the antinuclear antibodies were negative. Without a definitive diagnosis, the lesions were treated, elsewhere, with topical steroids. However, a complete remission was never achieved. Her medical history was significant for asthma and polyallergy (milk products, pet dander, house dust mites, molds, pollen). In addition, she experienced a benign breast adenoma, surgery for a myomatous uterus, cholecystolithiasis and a thyroid adenoma. She was regularly taking iodine (75 mg daily) and contraceptives. Otherwise, she was in good general condition. Her family history was unremarkable. Clinical Findings
On examination, erythematous, succulent, urticaria-like annular plaques with a smooth surface were observed on her neck, both shoulders and the right lateral aspect of her upper arm (Fig. 1). There was no regional lymphadenopathy.
| Fig. 1. A 47-year-old woman with annular, erythematous, urticaria-like plaques of lupus erythematosus tumidus (LET). |
 |

  |
Histopathology
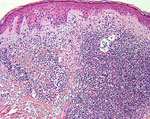
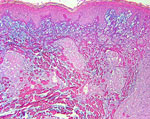
A lesional skin biopsy specimen showed a dense perivascular and periadnexal lymphocytic infiltration in the upper and middle dermis without epidermal involvement (Fig. 2). Colloidal iron staining revealed abundant interstitial mucin deposition between collagen bundles (Fig. 3). Direct immunofluorescence with anti-IgA and anti-IgG at dermoepidermal junction was negative.
| Fig. 2. LET: perivascular and periadnexal lymphocytic infiltration in the dermis without epidermal involvement ( HE x100). |
 |

  |
| Fig. 3. Colloidal iron staining shows an interstitial mucin deposition between collagen bundles in LET (x 100). |
 |

  |
Examination and Laboratory Findings
Laboratory findings, including complete blood cell count, electrolytes, liver and kidney function tests, C-reactive protein and thyroid hormones, were within normal ranges. Serum IgE (648 kU/l) and eosinophil cationic protein (37 µg/l) levels were slightly elevated. Serology for Lyme borreliosis was negative. Antinuclear antibodies (ANA) using HEp-2 cells were negative, and anti-dsDNA, anti-Ro/SSA and anti-Sm antibodies were not detected. Provocative phototesting showed no characteristic skin alterations with UV-B, a slight erythema with UV-A, and a strong persistent erythematous reaction with both UV-A and UV-B irradiation. Examination of biopsy specimens, obtained from phototesting area 1 week later, demonstrated characteristic histological findings consistent with LET. Staging, according to the American College of Rheumatology (ACR) criteria, showed no evidence of systemic involvement. Abdomen sonography revealed cysts in the right kidney and cholecystolithiasis. Diagnosis
Based on clinical and histological findings, as well as positive photosensitivity results, a diagnosis of LET was made. Therapy and Course
We treated our patient only with topical tacrolimus ointment 0.1% twice daily. Tacrolimus was tolerated well without side effects. After 4 weeks, she presented with a significant improvement of her lesions. Application of tacrolimus was continued once daily. After 12 weeks of therapy, the lesions completely subsided (Fig. 4). Regular use of a potent sunscreen was recommended.
| Fig. 4. LET lesions subsided after 12 weeks of treatment with topical tacrolimus ointment. |
 |

  |
Discussion
Cutaneous lupus erythematosus (CLE) is an autoimmune disease that has a wide spectrum of clinical manifestations. It may present as subacute (SCLE) type as well as chronic (CCLE) type, including discoid LE, chilblain LE, LE profundus and LE tumidus (LET). LET is a rare but distinct subtype of CCLE, characterized by erythematous, succulent, urticaria-like, non-scarring plaques in sun-exposed areas. It was first described in 1930 (1); however, reports on LET patients have become more frequent over the last few years. The pathogenesis of LET remains unclear. Its clinical appearance results from the excessive dermal deposition of mucin. A slight male predominance has been noticed in adults and antinuclear antibodies were detected in 10% of the patients with LET (2). Interestingly, LET has been reported also in childhood (3). Photosensitivity has been described to be very high in LET. Kuhn et al. reported that 72% of the patients with LET reacted to UV photoprovocation (4). Phototesting in large series of LE patients demonstrated that LET was the most UV-sensitive form of LE (70-80%), compared to SCLE (63%) and DLE (36%) (5). Since the characteristic histological changes of LET are not often prominent, its diagnosis may be difficult, as in our case. The differential diagnosis includes other subtypes of LE (discoid LE and SCLE), polymorphous light eruption, Jessner’s lymphocytic infiltration of the skin, pseudolymphoma, reticular erythematous mucinosis, and erythema annulare centrifugum. Antimalarials, systemic and topical corticosteroids are the most commonly used therapeutic regimens in LET. However, a long-term topical treatment with corticosteroids can lead to numerous side effects such as skin atrophy, telangiectasia, striae, senile-type purpura, hypertrichosis, rosacea-like dermatitis, perioral dermatitis, aggravation of preexisting folliculitis and dermatophyte infection, exacerbation of acne and glaucoma (6). Recently, several case reports on the topical immunomodulator tacrolimus (FK506) (7-9), as well as pimecrolimus (10), applied in systemic, subacute and discoid LE suggested a good therapeutic efficacy. Tacrolimus, as a single or adjunct agent, has been reported to be effective and well tolerated in LET (11). Interestingly, intraperitoneal tacrolimus has been shown to reduce lupus-like skin lesions in a murine model (12). Although the mechanism of tacrolimus action in LET is not completely understood, its antiinflammatory effect could be explained by the inhibition of calcineurin, resulting in suppression of antigen-presenting T cells, inhibition of the production and release of inflammatory cytokines including interleukins-2, -3 and -4, granulocyte colony-stimulating factor, tumor necrosis factor- αand interferon γ(13). Furthermore, tacrolimus has been reported to be effective in chronic inflammatory conditions such as severe and resistant atopic eczema, especially in facial lesions ofchildren, psoriasis, lichen planus, localized scleroderma, chronic actinic dermatitis, pyoderma gangrenosum, Behçet’s disease, dermatomyositis, rheumatoid ulcers and steroid rosacea (14-17). The common side effects of tacrolimus are burning sensation, itching or erythema, which usually ameliorate with continuation of treatment. Most important, tacrolimus does not cause skin atrophy, unlike topical corticosteroids, and its systemic absorption is minimal. In conclusion, we presented a woman with annular lesions of LET who was successfully treated with topical tacrolimus. Our case confirms that tacrolimus may be helpful in treating this rare skin condition. However, additional studies in a large group of patients are necessary to confirm our results. References
1. Gougerot, H., Burnier, R. Lupus érythémateux ‘tumidus’. Bull Soc Fr Dermatol Syphilol 1930, 37: 1291-2. 2. Kuhn, A., Richter-Hintz, D., Oslislo, C. et al. Lupus erythematosus tumidus: a neglected subset of cutaneous lupus erythematosus: report of 40 cases. Arch Dermatol 2001, 136: 1033-41. 3. Sonntag, M., Lehmann, P., Megahed, M., Ruzicka, T., Kuhn, A. Lupus erythematosus tumidus in childhood. Dermatology 2003, 207: 188-92. 4. Kuhn, A., Sonntag, M., Richter-Hintz, D. et al. Phototesting in lupus erythematosus tumidus - review of 60 patients. Photochem Photobiol 2001, 73: 532-6. 5. Walchner, M., Messer, G., Kind, P. Phototesting and photoprotection in LE. Lupus 1997, 6: 167-74. 6. Hill, C.J.H., Rostenberg, A. Adverse effects from topical steroids. Cutis 1978, 21: 624-8. 7. Bohm, M., Gaubitz, M., Luger, T.A., Metze, D., Bonsmann, G. Topical tacrolimus as a therapeutic adjunct in patients with cutaneous lupus erythematosus. A report of three cases. Dermatology 2003, 207: 381-5. 8. Lampropoulos, C.E., Sangle, S., Harrison, P., Hughes, G.R.V., D’Cruz, D.P. Topical tacrolimus therapy of resistant cutaneous lesions in lupus erythematosus: a possible alternative. Rheumatology 2004, 43: 1383-5. 9. Kanekura, T., Yoshii, N., Terasaki, K. et al. Efficacy of topical tacrolimus for treating the malar rash of systemic lupus erythematosus. Br J Dermatol 2003, 148: 353-6. 10. Kreuter, A., Gambichler, T., Breuckmann, F. et al. Pimecrolimus 1% cream for cutaneous lupus erythematosus. J Am Acad Dermatol 2004, 51: 407-10. 11. Bacman, D., Tanbajewa, A., Megahed, M., Ruzicka, T., Kuhn, A. Topical treatment of lupus erythematosus tumidus with tacrolimus. Hautarzt 2003, 54: 977-9. 12. Furukawa, F., Imamura, S., Takigawa, M. FK506: therapeutic effects on lupus dermatoses in autoimmune-prone MRL/Mp-lpr/lpr mice. Arch Dermatol Res 1995, 287: 558-63. 13. Nasr, I.S. Topical tacrolimus in dermatology. Clin Exp Dermatol 2000, 25: 250-4. 14. Lener, E.V., Brieva, J., Schachter, M. et al. Successful treatment of erosive lichen planus with topical tacrolimus. Arch Dermatol 2001, 137: 419-22. 15. Mancuso, G., Berdondini, R.M. Topical tacrolimus in the treatment of localized scleroderma. Eur J Dermatol 2003, 13: 590-2. 16. Petering, H., Kiehl, P., Breuer, C. et al. Pyoderma gangrenosum: successful topical therapy with tacrolimus (FK506). Hautarzt 2001, 52: 47-50. 17. Schuppe, H., Richter-Hintz, D., Stierle, H.E. et al. Topical tacrolimus for recalcitrant leg ulcer in rheumatoid arthritis. Rheumatology 2000, 39: 105-6. |