A Nonhealing Leg Ulcer
Matilda Bylaite and Thomas Ruzicka
Department of Dermatology, Heinrich-Heine-University Duesseldorf, Duesseldorf, Germany
History
An 85-year-old woman was referred with a 5-year history of a nonhealing ulcer on the right lower leg. The ulcer had not responded to consistent conservative treatment, compression therapy and split-thickness skin grafting. Her medical history was remarkable for chronic venous insufficiency and posttrombotic syndrome of the right lower leg. Additionally, she had hypertension, arrhythmia, myocardial hypertrophy, glaucoma and type 2 diabetes mellitus. Her medications included nitroglycerin, methyldigoxin, atenolol, amlodipine, aspirin and metformin. The patient denied any arsenic exposure, irradiation or burns. She had no positive history of skin cancer. Clinical Findings
Physical examination revealed a coin-shaped 4 x 4 cm ulcer on the medial pretibial aspect of her right lower leg (Fig. 1). The surface of the ulcer demonstrated shiny granulation tissue (Fig. 2). There were mild eczematous changes of the surrounding skin. One could also observe skin hyperpigmentation, edema and dilated tortuous veins on both lower legs and coronal phlebectasia around her ankles. Peripheral pulse was palpable. There was no inguinal or femoral lymphadenopathy.
| Fig. 1. Basal cell carcinoma presenting as pretibial ulcer of the right lower leg in the setting of chronic venous insufficiency. |
 |

  |
| Fig. 2. Ulcerating basal cell carcinoma of the lower leg showing shiny granulation tissue. |
 |

  |
Histopathology
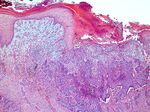
A biopsy specimen obtained from the edge and base of the ulcer revealed an ulcerated nodular basal cell carcinoma (Fig. 3).
| Fig. 3. Ulcerating nodular basal cell carcinoma of the lower leg (HE, x50). |
 |

  |
Examination and Laboratory Findings
Laboratory tests were within normal limits. Doppler-duplex sonography revealed bilateral superficial femoral, saphenous and popliteal venous reflux and deep vein thrombosis of the right leg. Computed tomography of right lower leg showed thickened medial pretibial skin without any infiltration or destruction of underlying tibia. Chest x-ray and abdomen sonography revealed no abnormal findings. Diagnosis
Based on histopathological findings, a diagnosis of ulcerated basal cell carcinoma of the right lower leg in association with chronic venous insufficiency was established. Therapy and Course
The patient was treated with an extensive excision. The affected area was covered with a split-thickness skin graft with complete healing occurring within 1 month. At 5-month follow-up, there was no sign of recurrence. Regular control and compression therapy were suggested. Discussion
Chronic venous ulcers of the lower leg, particularly in the medial malleolar area, are usually diagnosed without any difficulties as a manifestation of chronic venous insufficiency, especially when varicose veins and stasis changes are evident. Chronic leg ulcers, however, can be also a clinical presentation of carcinoma; in addition, carcinoma can be a complication of leg ulcers. Malignant transformation such as squamous cell carcinoma (SCC) and basal cell carcinoma (BCC) in the site of chronic ulceration has been previously considered to be a very rare complication of chronic deep venous insufficiency (1-4). Recent reports demonstrate that skin carcinomas, particularly BCC developing within leg ulcers are not as uncommon as we used to believe (5-11). Moreover, metastasizing BCC has also been reported in a stasis ulcer in a black woman (12). Although BCC is the most common skin cancer, often found on the sun exposed areas such as head and neck, in a small number of cases it arises on the lower extremities. Patients developing cancers in leg ulcers were usually women. The results from a large study in Australia showed that in 2.2 malignancies observed per 100 leg ulcers, 75% were BCC and only 25% were SCC (5). Whether there is an increased risk of developing BCC in chronic leg ulcers or it occurs as a primary skin cancer in association with venous insufficiency, remains unclear (6). Previous exposure to arsenic, excessive ultraviolet light irradiation, chronic infection, constant mechanical irritation or trauma of varying origin are known to be the most common co-carcinogenic factors. Black and Walkden noticed that BCCs on the lower legs had a tendency to ulcerate early, and suggested that chronic venous stasis may induce epidermal hyperplasia, which could lead to a development of BCC (7). In our case, as well as in most reported cases, it is difficult to say if our patient had a BCC as a complication of a leg ulcer or it developed de novo. Since BCC has a benign appearance, it is rarely considered in the differential diagnosis of leg ulcers. To distinguish BCC in the setting of chronic venous insufficiency and ulceration might be challenging, especially when the ulcer demonstrates a slow growth and has an appearance of healthy granulation tissue (8, 9). Therefore, biopsy should be performed in any leg ulcer that does not respond to traditional treatment modalities within 3 months (10) and has an atypical appearance or location. Usually, a number of skin biopsies are required to confirm the diagnosis. We present a patient with an ulcerating BCC on the lower extremity in association with chronic venous insufficiency. One should consider BCC in any leg ulcer that fails to heal especially when the ulcer is located at an atypical site for a venous or stasis ulcer (7). A skin biopsy to detect malignant transformation in nonhealing leg ulcers is essential to provide an adequate treatment. References
1. Knox, L.C. Epithelioma and chronic varicose ulcer. JAMA 1925, 85: 1046-50. 2. Black, W. Neoplastic disease occurring in varicose ulcers or eczema: a report of six cases. Br J Cancer 1952, 6: 120-6. 3. Burns, D.A., Calnan, C.D. Basal cell epithelioma in a chronic leg ulcer. Clin Exp Dermatol 1978, 3: 443-5. 4. Blank, A.A., Schnyder, U.W. Squamous cell carcinoma and basal cell carcinoma within the clinical picture of chronic venous insufficiency in the third stage. Dermatologica 1990, 181: 248-50. 5. Yang, D., Morrison, B.D., Vandongen, Y.K. et al. Malignancy in chronic leg ulcers. Med J Aust 1996, 164: 718-20. 6. Granel, F., Barbaud, A., Schmutz, J.L. Basal and squamous cell carcinoma associated with chronic venous leg ulcer. Int J Dermatol 2000, 39: 78-9. 7. Black, M.M., Walkden, V.M. Basal cell carcinomatous changes on the lower leg: a possible association with venous stasis. Histopathology 1983, 7: 219-27. 8. Harris, B., Eaglstein, W.H., Falanga, V. Basal cell carcinoma arising in venous ulcers and mimicking granulation tissue. J Dermatol Surg Oncol 1993, 19: 150-2. 9. Lutz, M.E., Davis, M.D.P., Otley, C.C. Infiltrating basal cell carcinoma in the setting of a venous ulcer. Int J Dermatol 2000, 39: 519-20. 10. Phillips, T.J., Salman, S.M., Rogers, G.S. Nonhealing leg ulcers: A manifestation of basal cell carcinoma. J Am Acad Dermatol 1991, 25: 47-9. 11. Schwarze, H.P., Loche, F., Gorguet, M.C., Kuchta, J., Bazex, J. Basal cell carcinoma associated with chronic venous leg ulcer. Int J Dermatol 2000, 39: 75-80. 12. Lanehart, W.H., Sanusi, I.D., Misra, R.P., O’Neal, B. Metastasizing basal cell carcinoma originating in a stasis ulcer in a black woman. Arch Dermatol 1983, 119: 587-91. |