Acute Generalized Exanthematous Pustulosis due to Amoxicillin
Matilda Bylaite and Thomas Ruzicka
Department of Dermatology, Heinrich-Heine-University Duesseldorf, Duesseldorf, Germany
History
A 46-year-old woman developed high fever and a widespread pruritic, erythematous pustular rash 4 days after taking antibiotics for an exacerbation of chronic maxillary sinusitis. Initially, oral cephalosporin was prescribed. Three days later, as there was no clinical improvement of sinusitis, amoxicillin was started. Twelve hours later, the patient noticed severe facial flushing. The next day she developed a pruritic erythematous eruption over her face, trunk and extremities with rapidly spreading pustules. Antihistamines and a single dose of oral prednisone 60 mg did not provide any relief. Within the next 2 days, the temperature rose over 39°C, her face and small joints became swollen, and she referred to the emergency room of our clinic. An adverse drug reaction was suspected and the patient was admitted to the hospital for further treatment. Her medical history included hay fever, induced by pollen and cat dander. Besides this, she was healthy and had no personal or family history of psoriasis. Clinical Findings
Physical examination revealed generalized, numerous, tiny 1-2 mm, monomorphic, yellow pustules on erythematous and edematous base, mainly located on her face, especially forehead and cheeks, neck, décolleté region and back (Fig. 1). Small solitary pustules were also noticed on the scalp and extremities. Facial edema and symmetric swelling of the hands and feet were evident. The oral mucosa, palms and soles were spared. The temperature was 39.6°C.
| Fig. 1A: Acute generalized exanthematous pustulosis (AGEP). A 47-year-old woman with numerous, tiny, monomorphic, nonfollicular yellow sterile pustules arising on widespread erythematous background on her face. |
 |

  |
| Fig. 1B: Acute generalized exanthematous pustulosis (AGEP). A 47-year-old woman with numerous, tiny, monomorphic, nonfollicular yellow sterile pustules arising on widespread erythematous background neck and décolleté region. |
 |

  |
| Fig. 1C: Acute generalized exanthematous pustulosis (AGEP). Close view showing sterile pustules on an erythematous background in a 47-year-old woman. |
 |

  |
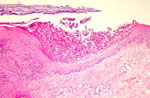
Histopathology
A skin biopsy from a pustular lesion from the back showed mild spongiosis, subcorneal collections of neutrophils, moderate papillary dermal edema and a superficial perivascular infiltrate of lymphocytes, neutrophils and eosinophils (Fig. 2). The histopathologic findings were consistent with a pustular drug eruption.
| Fig. 2: Histopathology of acute generalized exanthematous pustulosis (AGEP). Mild spongiosis, subcorneal collections of neutrophils, moderate papillary dermal edema and a superficial perivascular mixed cell infiltrate, hematoxylin-eosin staining. |
 |

  |
Examination and Laboratory Findings
Hemogram revealed a leukocyte count of 9800/mm3 and mild microcytic anemia. CRP was slightly elevated. Results of other laboratory tests, including routine blood biochemistry, penicillin-RAST (Penicilloyl G, Penicilloyl V, Ampicilloyl and Amoxicilloyl) were within normal limits and nondiagnostic. The culture from pustules was sterile. ENT consultant confirmed an exacerbation of chronic maxillary sinusitis and prescribed symptomatic treatment. Diagnosis
The diagnosis of an acute generalized exanthematous pustulosis (AGEP) induced by amoxicillin was established based on the history, clinical manifestation and histopathologic and laboratory findings. Therapy and Course
As expected, withdrawal of amoxicillin and treatment with systemic corticosteroids, antihistamines and topical corticosteroids led to rapid resolution of the pustular eruption within 1 week (Fig. 3). Oral prednisone 100 mg as initial daily dose followed by gradual tapering was prescribed. Symptomatic treatment for sinusitis was also continued. Within the few first days the skin lesions became confluent and livid and exhibited a predominantly targetoid pattern on extremities. Our patient was discharged with remarkable improvement with only mild postinflammatory hyperpigmentation on lower extremities on day 10 on prednisone 30 mg/daily, which was discontinued later with no recurrence of her skin eruption.
| Fig. 3: Complete resolution within 10 days after withdrawal of antibiotics and short course of prednisone. |
 |

  |
Discussion
Acute generalized exanthematous pustulosis (AGEP) is an uncommon skin reaction, characterized by an acute self-limited erythematous pustular eruption, mostly (90%) caused by drugs. For years, this disorder has been erroneously classified as von Zumbusch-type pustular psoriasis. In 1980, Beylot introduced the term of AGEP, and few years later the drugs in its etiology were assessed (1, 2). Recently, the main characteristics of AGEP, acute, extensive formation of numerous, small, pinhead-sized, mostly nonfollicular sterile pustules, arising on widespread erythematous background, associated with high fever (38°C) and peripheral blood leukocyte count higher than 7000/mm3, were proposed. Histopathology reveals subcorneal or intraepidermal pustules, dermal edema, vasculitis, perivascular eosinophils and/or focal necrosis of keratinocytes (3). In particular, antibacterials such as ß-lactams and macrolides have been implicated in the majority of AGEP cases (2). In our case, amoxicillin was believed to be the causative agent. Other drugs, such as antipyretics, analgetics, calcium channel blockers, antiarrhythmics, anxiolytics, tricyclic antidepressants and antimycotics, can also induce pustular eruption (4). Other factors affecting the immune system, including acute infections (enterovirus or parvovirus B19), heavy metals (mercury) and radiation have also been implicated (3). Nevertheless, in about 5% of AGEP cases no etiology could be identified (2). Although the pathogenesis of AGEP remains uncertain, recent data report the involvement of a drug-specific CD4 and CD8 immune reaction, which results in a preferential interleukin (IL)-8 production by T cells (5). The involvement of T cells in AGEP can be implied by positive skin patch tests and lymphocyte transformation tests. The differential diagnosis of AGEP includes a wide range of diseases or reactions that can cause pustular eruptions of the skin, like generalized von Zumbusch-type pustular psoriasis, subcorneal pustulosis of Sneddon-Wilkinson, atypical Sweet syndrome, acute infectious generalized pustulosis, generalized candidiasis, eosinophilic pustular folliculitis (Ofuji) and others (4). The most important aspect of AGEP management is the immediate withdrawal of the suspected drug. Although it is a self-limited condition with resolution of pustules within less than 15 days, systemic and topical corticosteroids are often employed in severe cases (3). Herein we describe an interesting case of acute generalized pustular eruption induced by amoxicillin. Early diagnosis of AGEP will facilitate exclusion of acute generalized pustular psoriasis or generalized infections, allowing adequate treatment. References
1. Beylot, C., Bioulac-Sage, P., Doutre, M.S. et al. Poustuloses exanthématiques aïgues généralisées. A propos de 4 cas. Ann Dermatol Venereol 1980, 107: 37-48.
2. Roujeau, J.C., Bioulac-Sage, P., Bourscau, C. et al. Acute generalized exanthematous pustulosis. Analysis of 63 cases. Arch Dermatol 1991, 127: 1333-8.
3. Roujeau, J.C. Neutrophilic drug eruptions. Clin Dermatol 2000, 18: 331-7.
4. Rogalski, C., Hürlimann, A., Burg, G. et al. Arzneimittelreaktion auf Terbinafin unter dem Bild einer akuten generalisierten exanthematischen Pustulose (AGEP). Hautarzt 2001, 52: 444.
5. Britschgi, M., Steiner, U.C., Schmid, S. et al. T-cell involvement in drug-induced acute generalized exanthematous pustulosis. J Clin Invest 2001, 107: 1433-41. |