Disseminated Superficial Actinic Porokeratosis
Matilda Bylaite and Thomas Ruzicka
Department of Dermatology, Heinrich-Heine-University Duesseldorf, Duesseldorf, Germany
History
A 55-year-old white woman presented to our out-patient department with a 4-year history of an asymptomatic eruption on her lower extremities. The number and size of the lesions have been increasing gradually over the last years. Multiple actinic keratoses were diagnosed by her dermatologist, and she had been treated with various topical glucocorticoids, retinoic acid and the frequency-doubled Nd:YAG laser without benefit. Her medical history included arrhythmias and regular use of digoxin, acetylsalicylic acid and diuretics for the last 3 years. There was no history of excessive sun exposure. There was no family history of skin diseases. Clinical Findings
Skin examination revealed type II skin with multiple, annular, variable-sized, well-defined, erythematous plaques and papules with elevated hyperkeratotic borders and an atrophic center (Fig. 1 A, B, C). The lesions were symmetrical and mainly located on the legs and buttocks. Few discrete lesions were also observed on her forearms, back and lower abdomen. Some papules around her knees and on the buttocks were fully covered with yellowish crust. Visibly and palpably enlarged varicose superficial veins were noticed in her lower legs.
| Fig. 1A. Disseminated superficial actinic porokeratosis in lower extremities. |
 |

  |
| Fig. 1B. Disseminated superficial actinic porokeratosis on the buttocks. |
 |

  |
| Fig. 1C. Disseminated superficial actinic porokeratosis. Flat papules with well-defined, slightly raised, keratotic margins and atrophic center. |
 |

  |
Histopathology
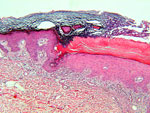
A biopsy specimen of a papule with raised hyperkeratotic ridge revealed an atrophic epidermis with an epidermal keratin-filled invagination and over-rising parakeratotic column, the so-called cornoid lamella (Fig. 2). Beneath the cornoid lamellae, the granular layer was absent, and the keratinocytes were vacuolated, dyskeratotic and disorganized. In the dermis, a mild lymphohistiocytic infiltration was observed. A histologic diagnosis of porokeratosis was made.
| Fig. 2. Disseminated superficial actinic porokeratosis. Characteristic cornoid lamella over an absent granular layer with vacuolated and dyskeratotic keratinocytes (HE x100). |
 |

  |
Examination and Laboratory Findings
Laboratory results were within normal limits. Diagnosis
Based upon clinical and histological features the diagnosis of disseminated superficial actinic porokeratosis was established. Therapy and Course
The lesions were treated with topical salicylic acid and lactic acid ointments with slight improvement. Cryotherapy is planned as a therapeutic option. Discussion
The porokeratoses are defined as specific disorders of keratinization and include five clinical variants, such as plaque-type porokeratosis of Mibelli, linear porokeratosis, disseminated superficial porokeratosis, porokeratosis palmaris, plantaris et disseminata, porokeratosis punctata palmaris et plantaris, and the most common, disseminated superficial actinic porokeratosis (DSAP). DSAP is an autosomal dominant cutaneous disorder characterized by multiple, small, annular, slowly expanding keratotic plaques, with raised, hyperkeratotic borders and central atrophy, erythema or pigmentation. The lesions develop predominantly on sun-exposed areas, such as the extensor surfaces of the legs and arms, with relative sparing of the face (1). Typically, DSAP manifests by the third and fourth decades, and exacerbates during summer or after phototherapy (1). It is usually asymptomatic; however, pruritus or stinging might be experienced. The histopathological hallmark of DSAP is the so-called cornoid lamella, a column of parakeratosis. Below it, the granular layer is absent and the keratinocytes are irregularly arranged and have pyknotic nuclei with perinuclear edema (1). A sparse lymphocytic infiltrate presents in the upper part of the dermis. The lesions may be mistaken for multiple actinic keratoses, stucco keratoses, atrophic annular lichen planus, flat seborrheic keratoses or disseminated granuloma annulare.The etiology of DSAP is unclear. Risk factors for the development of DSAP include genetic inheritance, immunosuppression and ultraviolet radiation (1). It has been suggested that local or systemic immune suppression may allow the development of mutant clones of keratinocytes (2). Recently, mutations in the p53 gene have been reported in porokeratosis, which may play a role in malignant transformation (3). The association between renal transplantation and porokeratosis has been noticed (4). Although the lesions of DSAP do not develop into a cancer as frequently as other types of porokeratosis, several reports on squamous cell carcinoma and Bowen’s disease developing within DSAP suggest that it may be premalignant (5).Various treatment modalities have been tried in DSAP, with variable results. The disease is difficult to treat, although cryotherapy, 5-fluorouracil and retinoic acid have been often used. Topical corticosteroids, vitamin D3 analogues, such as tacalcitol and calcipotriol, and also systemic retinoids or corticosteroids have been reported to be effective in DSAP and other porokeratoses (6). As there is a risk for malignant transformation of DSAP lesions, patients should be advised to avoid excessive ultraviolet radiation, to use sun protection, emollients and visit a dermatologist for periodic examination. References
1. Chernosky, M.E., Freeman, R.G. Disseminated superficial actinic porokeratosis. Arch Dermatol 1967, 96: 611-24.
2. Reed, R.J., Leone, P. Porokeratosis: A mutant clonal keratosis of the epidermis. I. Histiogenesis. Arch Dermatol 1970, 101: 340-7.
3. Magee, J.W., McCalmont, T.H., LeBoit, P.E. Overexpression of p53 tumor suppressor protein in porokeratosis. Arch Dermatol 1994, 130: 187-90.
4. Herranz, P., Pizarro, A., De Lucas, R. et al. High incidence of porokeratosis in renal transplant recipients. Br J Dermatol 1997, 136: 176-9.
5. Leache, A., Soto de Delas, J., Vazquez Doval, J., Lozano, M.D., Quintanilla, E. Squamous cell carcinoma arising from a lesion of disseminated superficial actinic porokeratosis. Clin Exp Dermatol 1991, 16: 460-2.
6. Bohm, M., Luger, T.A., Bonsmann, G. Disseminated superficial actinic porokeratosis: Treatment with topical tacalcitol. J Am Acad Dermatol 1999, 40: 479-80. |